Novel therapies for Muscular Dystrophy
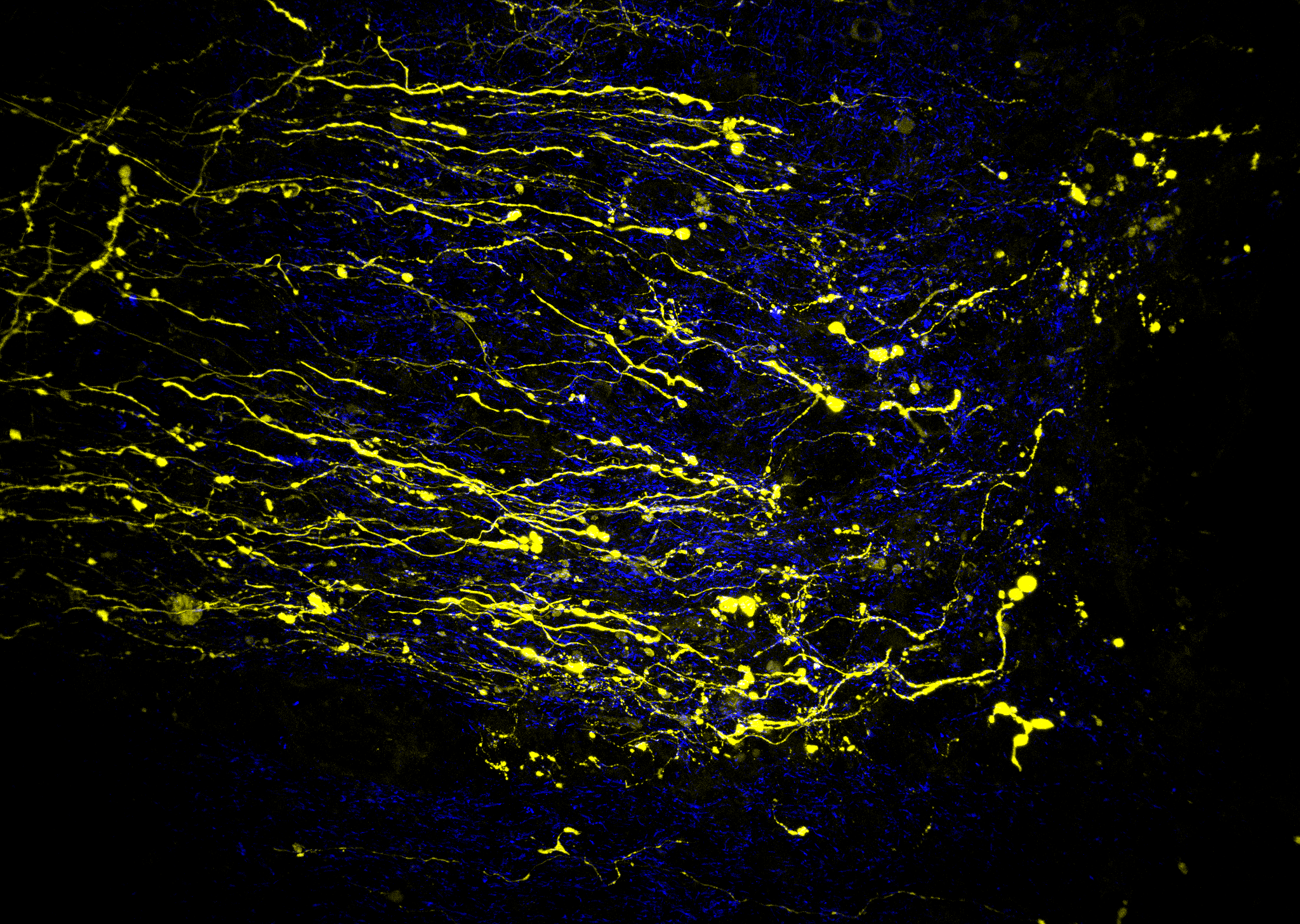
Duchenne muscular dystrophy (DMD) is the most common and sever neuromuscular disease affecting children. DMD is an X-linked recessive disease affecting mostly boys, with a prevalence of 1:5000 male births worldwide. DMD is caused by mutations in the dystrophin gene, which encodes a large, membrane-localized protein found predominantly in skeletal and cardiac muscle but also in smooth muscle and some areas of the brain. A key finding of my early research was that the increased membrane permeability in mdx (DMD) mice was largely due to the downstream effects of excessive calcium influx through stretch-activated ion channels and increased reactive oxygen species (ROS) production, and not due to mechanical tearing of the membrane, as was originally proposed. These results highlighted the important signaling role of the dystrophin complex. A follow up study showed that NADPH oxidase 2 (NOX2) was the major source of oxidative stress in mdx muscle, which also triggered the calcium influx through stretch-activated channels. This result provided a new therapeutic target for DMD. This research led to a study showing that simvastatin, a commonly used cholesterol lowering drug, dramatically improves skeletal muscle function in dystrophic mice, and identified inhibition of NOX2-derived ROS as an important mechanism underlying the benefits provided by simvastatin. A follow up study demonstrated that simvastatin also significantly improves cardiac function in mdx mice.
In last few years, my research has focused on developing a novel gene therapy approach for DMD. Due to the enormous size of the dystrophin gene, only about one third will fit into the most commonly used gene delivery vector, adeno-associated virus (AAV). In addition to size constraints, AAV also has other limitations, including lack of tissue-specific targeting and likely immunogenicity from repeat doses. Therefore, my goal was to design a non-viral gene delivery platform with three key characteristics to overcome the limitations of AAV. Firstly, I developed antibodies against a muscle protein, which allows binding and uptake of the non-viral gene platform into skeletal and cardiac muscle. Secondly, the platform is able to accommodate large genes, including the full-length Dystrophin gene. Finally, since the platform is completely non-viral, the possibility of immunogenicity is dramatically reduced and hopefully this will allow for repeat dosing over months or years. Stan Froehner and I are the co-founders of Myosana Therapeutics, a University of Washington spinout, which is currently developing our non-viral gene therapy platform, with the ultimate aim of producing a potential therapy for DMD and other muscle diseases.